Everything Worth Knowing About Antibiotic Resistance
Antibiotic resistance arises when bacteria evolve and become resistant to the antibiotic drugs that usually kill them. Here is everything worth knowing about antibiotic resistance.
Antibiotic resistance severely restricts available treatments and is a major global health issue. Some bacteria strains are now considered superbugs, implying they resist various antibiotics.
What Is Antibiotic Resistance?
The ability of bacteria to withstand the effects of antibiotics, a class of medication like penicillin or ciprofloxacin that kills or slows the growth of germs, is known as antibiotic resistance. Antibiotic-resistant bacteria restrict the range of available treatments and make treating diseases brought on by those germs more challenging.
Alternative therapies could be expensive and even harmful in some situations. Drugs used to treat other microbes may also cause them to develop treatment resistance. Bacteria are resistant to antibiotics, while most other microbes are not.
For instance, fungi and viruses can both acquire resistance to antiviral and antifungal medications. The generic phrase to describe a microorganism’s resistance to drugs used to cure disease is “antimicrobial resistance.”
Sometimes referred to as “superbugs,” microorganisms that acquire medication resistance. Some infectious disorders that were previously under control can re-emerge because some infections are resistant to successful treatment with current drugs.
What Causes Antibiotic Resistance?
The following elements frequently fuel antibiotic resistance:
● Overuse of Antibiotics
Antibiotic resistance is a result of the overuse and misuse of antibiotics. For instance, viruses typically cause pharyngitis (sore throat). Antibiotics are useless. Without medications, even bacterial ear infections frequently get better.
● Misuse of Antibiotics
Bacteria take advantage of every chance to grow. Bacteria begin to multiply if you skip taking a medication for a day or several days, discontinue therapy too soon, or use the wrong antibiotics, like taking someone else’s prescription. They might alter as they grow in number (mutate). The medication becomes increasingly less effective against mutated microorganisms.
● Agricultural Use
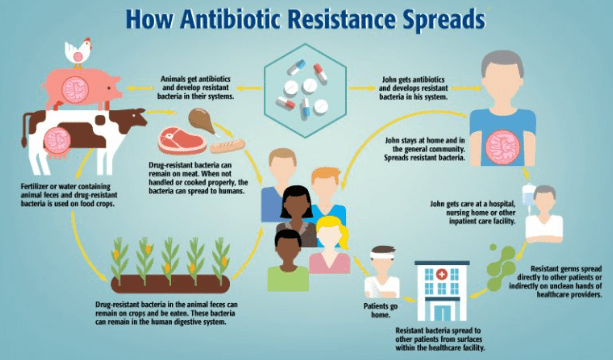
Animals can develop bacteria that are resistant to antibiotics. According to estimates, livestock in the US uses antibiotics 80% of the time.
● Spontaneous Resistance
A bacterium’s genetic makeup (DNA) can occasionally modify or alter. The antibiotic cannot effectively target this newly changed bacterium because it does not recognize it. Or the alteration aids the bacteria in fending off the effects of the medication.
● Transmitted Resistance
A contagious, antibiotic-resistant bacterial infection can be transmitted to another person. That person currently has a condition that is resistant to antibiotic treatment. Once more, we can typically discover a solution. The bacteria may be more challenging to treat now that they are immune because of time.
Who Is at Risk for Antibiotic Resistance?
Antibiotic resistance is more likely to occur as more individuals use them. Antibiotics are occasionally used by persons who don’t require them. Antibiotics, for instance, are ineffective against viruses.
Similar to bacteria, viruses are microscopic organisms that can enter your body and infect you. A virus can cause the common cold or the flu. In certain situations, using an antibiotic does not cure the illness. It might make antibiotic resistance more likely.
The danger also rises if an antibiotic is not fully consumed. You might not completely eradicate all the bacteria if you stop taking it too soon. The surviving microbes might develop resistance.
How Are Bacterial Infections Resistant to Antibiotics Treated?
Other varieties of antibiotics are used to treat illnesses that are resistant to antibiotics. Based on the sort of illness you have and the kinds of therapies the organism reacts to, your NYU Langone doctor recommends these medicines. It is possible to administer antibiotics intravenously (IV) or orally. In the hospital, at home, or in a rehabilitation center, IV antibiotics can be issued. Doctors occasionally recommend drug combinations.
A 7–10 day treatment of an antibiotic, such as doxycycline, clindamycin, or a mix of sulfamethoxazole-trimethoprim and linezolid, is frequently used to treat an MRSA infection at home.
The use of specific antibiotics such as polymyxin B, tigecycline, and beta-lactam combo antibiotics may be used to treat a patient with a disease caused by the carbapenem-resistant Enterobacteriaceae. It’s possible to need medication for a few days or up to six to eight weeks.
Depending on the kind of illness and where it is located in the body, the course of therapy may take some time.
For instance, the course of treatment for endocarditis, an infection of the heart’s inner lining, could continue up to six weeks. However, therapy for a urinary tract infection might last three days.
It is essential to adhere to your doctor’s recommendations when taking an antibiotic to minimize recurrence and the emergence of resistant bacteria. Even if you feel better after a few days, take your medication according to the prescribed schedule and complete the entire course of treatment.
Antibiotic Resistance: A Public Health Concern
According to the Centers for Disease Control and Prevention, more than 2 million Americans get sick with antibiotic-resistant infections yearly, and at least 23,000 pass away.
Antibiotic resistance is referred to as a public health issue by organizations like the National Institutes of Health and the Centers for Disease Control and Prevention. For patients and families, antimicrobial resistance can be expensive and distressing.
Drug-resistant infections can result in more prolonged hospital admissions, more follow-up doctor visits, and the need for potentially harmful and costly therapies.
Antibiotic effectiveness decreases as antibiotic resistance increases. To tackle the resistant germs, new treatments must be created. Assume that there are no new medications to combat the bacterium.
Therefore, it is crucial that people use antibiotics only when necessary and that hospitals and healthcare systems implement antimicrobial stewardship programs. Otherwise, therapy may be impossible.
The National Institutes of Health (NIH) has committed to addressing this public health issue by emphasizing infection prevention strategies, monitoring bacterial resistance, reserving our most potent antibiotics for patients with immunological disorders, and encouraging the discovery of novel antibiotics.
Conclusion
Your doctor may try a new medication if an illness displays antibiotic resistance. Testing different medicines increase the danger of antibiotic resistance, and the latest treatment may have more severe adverse effects.
For patients and families, antimicrobial resistance can be expensive and distressing. Drug-resistant infections can result in more prolonged hospital admissions, more follow-up doctor visits, and the need for potentially harmful and costly therapies.
Antibiotic effectiveness decreases as antibiotic resistance increases. To tackle the resistant germs, new treatments must be created. Assume that there are no new medications to combat the bacterium.
It is crucial for people to use antibiotics only when necessary and for hospitals and healthcare systems to put antimicrobial stewardship policies in place because therapy might be impossible otherwise.
Do not be afraid to reach out to me, Mark E Wilkins, to assist you in any issues you might have. Most Hypnotherapy sessions last 2 hours and EFT Sessions are usually handled with one session.
To make an appointment, first listen to the Pre-talk and fill out he Complementary Healthcare Provider Disclosure. The use the Contact Form to request an appointment with the Bohol Hypnosis Expert.




