Antibiotic resistance has escalated into a global crisis due to overuse in both healthcare and agriculture, coupled with the rapid spread of resistant strains. Effective strategies, including stringent antibiotic stewardship and enhanced public health education, are essential for managing this threat. Research into innovative treatments such as phage therapy and CRISPR-Cas technologies offers hope for sustainable solutions. Further exploration reveals the necessity of thorough approaches to adequately confront the ongoing challenge of antibiotic resistance.
Key Takeaways
- Implement antibiotic stewardship programs to guide proper use and minimize unnecessary prescriptions in healthcare settings.
- Reform agricultural antibiotic policies to balance animal health with preventing resistance spread in humans.
- Develop and promote novel antibiotics and alternative therapies, such as phage and peptide treatments, to address resistant bacterial strains.
- Educate medical professionals and the public on the risks of antibiotic misuse and the importance of adherence to prescribed treatments.
- Enhance infection prevention strategies to reduce the reliance on antibiotics and limit the development of resistance.
Understanding the Mechanics of Antibiotic Resistance
While antibiotic resistance is a well-recognized public health threat, the underlying mechanisms by which bacteria develop resistance are complex and multifaceted.
Bacterial mutations play a central role in these resistance mechanisms. These mutations may occur spontaneously or be induced by exposure to antibiotics, leading to genetic changes that confer survival advantages.
For instance, bacteria can develop efflux pumps that actively expel antibiotic molecules from their cells, or modify their target sites so antibiotics can no longer bind effectively.
Each mutation not only contributes to resistance against specific antibiotics but can also provide a blueprint for other bacteria, enhancing the spread of resistance.
The Role of Agricultural Practices in Escalating Resistance
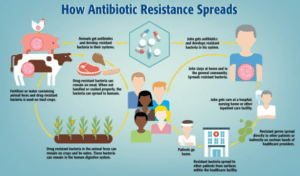
Understanding the genetic mechanisms of bacterial resistance provides a foundation for addressing another significant contributor to this dilemma: agricultural practices.
Extensive farm antibiotic use for livestock health enhancement and disease prevention has escalated resistance profiles among bacterial populations. Research consistently shows that antibiotics administered to animals can lead to resistant bacterial strains, which may transfer to humans through direct contact or consumption of animal products.
This cycle not only undermines antibiotic efficacy but also threatens global health security. Mitigating such risks requires a critical review and reform of current agricultural antibiotic policies to balance necessary animal healthcare with public health interests.
Strategies to Combat Antibiotic Misuse in Healthcare

To address the escalating issue of antibiotic misuse in healthcare settings, it is imperative to implement targeted strategies that enforce prudent use of these critical medications.
Effective antibiotic stewardship programs are essential, promoting adherence to evidence-based prescribing guidelines. These guidelines help healthcare providers determine the most appropriate antibiotic type, dosage, and duration for specific infections, reducing unnecessary prescriptions.
Regular training sessions for medical staff can reinforce the importance of these protocols and update them on the latest advancements in antibiotic resistance.
Additionally, monitoring and feedback mechanisms should be established to track antibiotic use and outcomes, ensuring continuous improvement in prescribing practices.
Exploring the Impact of Antibiotic Resistance on Public Health
Building on the importance of antibiotic stewardship discussed earlier, the public health implications of antibiotic resistance are profound and far-reaching.
Effective antibiotic stewardship programs, which encourage judicious antibiotic use, are critical to curbing the spread of resistance. These programs also emphasize robust infection prevention strategies, such as hygiene practices and vaccination, to reduce the need for antibiotics.
The rise in drug-resistant infections complicates treatment protocols, extends hospital stays, and increases mortality rates. Implementing thorough strategies that include both antibiotic stewardship and infection prevention is essential to mitigate the impact of antibiotic resistance on public health.
Innovations and Advances in Antibiotic Treatments

As the challenge of antibiotic resistance escalates, researchers and pharmaceutical companies are fervently pursuing innovative treatments and advances in antibiotic therapies. Development includes novel antibiotics and treatment alternatives, focusing on mechanisms that circumvent traditional resistance pathways. For instance, phage therapy utilizes bacteriophages to target specific bacterial strains, providing a promising alternative to conventional antibiotics.
| Innovation Type | Description | Status |
|---|---|---|
| Novel Antibiotics | Targets unexplored bacterial processes | Clinical trials |
| Phage Therapy | Uses viruses to destroy bacteria | Research phase |
| Peptide Therapeutics | Mimics immune system peptides | Early development |
| CRISPR-Cas Technology | Edits bacterial DNA to remove resistance | Experimental |
| Bacteriocin Application | Employs bacterial toxins against pathogens | Investigational |
This table highlights key innovative strategies being explored to combat antibiotic resistance.
The Importance of Global Cooperation in Addressing Resistance
Innovative solutions such as phage therapy and CRISPR-Cas technologies highlight the ongoing battle against antibiotic resistance, yet the scale of this crisis necessitates a unified global response.
International collaboration is essential, integrating diverse technological, scientific, and policy-driven approaches to stymie the spread of resistance.
Effective global surveillance systems are vital for detecting and tracking resistant strains, facilitating timely data sharing and coordinated response strategies.
This approach enables the adaptation of interventions based on real-time information, optimizing resource allocation and enhancing the efficacy of preventative measures, thereby preserving the utility of antibiotics for future generations.
Educating the Public and Healthcare Providers on Resistance Management

To effectively manage antibiotic resistance, educating both the public and healthcare providers is imperative. Public awareness campaigns are essential for informing individuals about the proper use of antibiotics and the risks associated with misuse.
Healthcare education programs must emphasize evidence-based practices for prescribing antibiotics. Key strategies include:
- Public Workshops: Interactive sessions to demonstrate the impact of antibiotic resistance.
- Healthcare Seminars: Focused training on diagnostic stewardship and infection control.
- Educational Materials: Distribution of guidelines and best practices for antibiotic use to both communities and medical institutions.
These efforts are critical to curb the spread and impact of antibiotic-resistant infections.
Frequently Asked Questions
How Does Antibiotic Resistance Affect Natural Ecosystems?
Antibiotic resistance disrupts natural ecosystems by causing imbalances, impacting wildlife health. Resistant bacteria can spread, altering microbial communities and potentially increasing disease susceptibility in various species, thereby disrupting ecological stability and biodiversity.
Can Probiotics Help Combat Antibiotic Resistance?
Steering through the labyrinth of microbial health, probiotics may offer benefits by bolstering gut health and potentially mitigating antibiotic resistance, but evidence remains mixed and further rigorous scientific investigation is essential to substantiate such claims.
What Are Common Myths About Antibiotic Resistance?
Common myths about antibiotic resistance include the belief that individuals, not communities, develop resistance and that overprescribing antibiotics does not impact public awareness and education about the broader implications of antimicrobial resistance.
How Does Antibiotic Resistance Affect Surgery Outcomes?
Antibiotic resistance complicates surgical outcomes by increasing the risk of postoperative infections. Resistant bacteria can prolong patient recovery, necessitate additional treatments, and raise healthcare costs, thereby challenging the effectiveness of standard prophylactic antibiotic protocols.
Are There Any Dietary Changes That Can Reduce Antibiotic Resistance Risks?
Dietary changes, such as increasing fermented foods and adopting plant-based diets, may influence gut microbiota and potentially reduce antibiotic resistance risks by promoting beneficial bacteria and decreasing the necessity for antibiotics.
Conclusion
In the battle against antibiotic resistance, the world stands at a crossroads akin to a sinking ship with a dwindling number of lifeboats. Each misuse of antibiotics is akin to drilling another hole in the hull, hastening the descent into the icy waters of unmanageable disease. Scientifically, every 1% increase in resistance can lead to thousands of deaths globally. This urgent crisis demands a unified, informed response to patch the breaches and keep humanity afloat.